A Comprehensive Guide to DMDD Treatment Options for Parents
Navigating treatment options for Disruptive Mood Dysregulation Disorder (DMDD)
9/14/20254 min read
Summary
As a parent of a child with Disruptive Mood Dysregulation Disorder (DMDD), navigating treatment options can feel overwhelming. This blog consolidates the latest research on DMDD treatments, including therapies, medications, and multimodal approaches, tailored for parents seeking clarity. We cover descriptions, effectiveness, side effects, and age suitability, with a focus on how these options may apply when DMDD co-occurs with Autism Spectrum Disorder (ASD). This is not medical advice always consult a qualified mental health professional for your child’s care. Our goal is to provide a clear, evidence-based resource to help you understand your options and ask informed questions.
Understanding DMDD and Its Challenges
If your child has been diagnosed with Disruptive Mood Dysregulation Disorder (DMDD), you’re likely familiar with their intense temper outbursts and chronic irritability. These behaviors, which often appear disproportionate to the situation, can disrupt family life, school, and friendships. DMDD is a mental health condition typically diagnosed in children ages 6 to 18, characterized by frequent outbursts (three or more times per week) and persistent irritability most of the day, nearly every day.
When DMDD co-occurs with Autism Spectrum Disorder (ASD), distinguishing between mood-driven outbursts and sensory-related meltdowns can make finding the right treatment even more complex.
This blog is designed for parents like you, struggling to gather reliable, up-to-date information in one place. Below, we’ve compiled a detailed guide to DMDD treatment options, including therapies, medications, and combined approaches. Each section includes research-backed effectiveness, potential side effects, suitable age ranges, and resources for further reading. This information is current as of September 14, 2025, and draws from trusted sources like the National Institute of Mental Health (NIMH), peer-reviewed studies, and clinical guidelines.
Please note: This is not a substitute for professional medical advice. Always work with your child’s doctor or mental health specialist to create a tailored treatment plan.
Treatment Options for DMDD: What Parents Need to Know
1. Cognitive Behavioral Therapy (CBT)
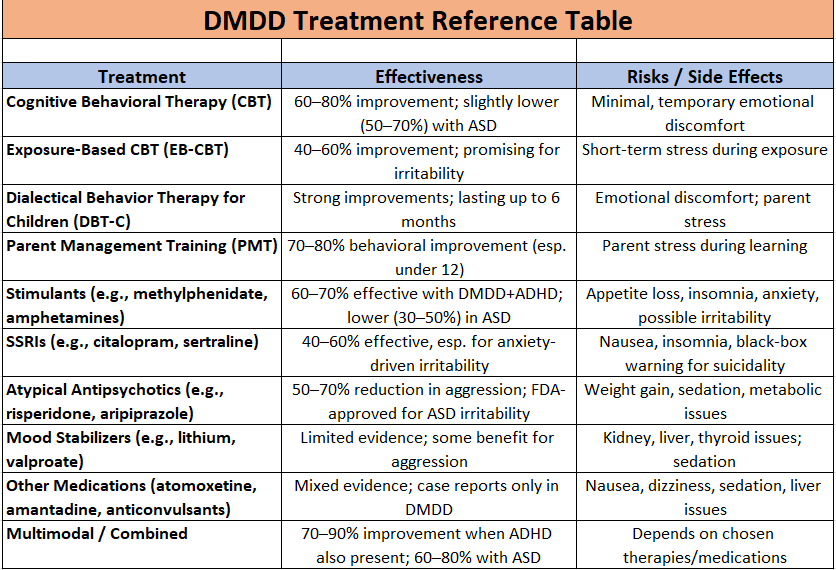
What It Is: CBT is a structured therapy that helps children identify negative thoughts, manage emotions, and develop coping skills to handle frustration and irritability. It often includes parent training to reinforce these skills at home. For children with both DMDD and ASD, CBT may be adapted to address social communication challenges.
Does It Work?
Research shows CBT reduces irritability and outbursts in many DMDD cases, with moderate to large improvements. One study found 60–80% of children showed measurable progress (PMC article). For kids with both ASD and DMDD, effectiveness drops slightly because irritability may also stem from sensory overload.
Side Effects: Minimal. Children may feel temporary emotional discomfort during sessions, but there are no physical side effects.
Best for Ages: 7–17.
Resources:
2. Exposure-Based Cognitive Behavioral Therapy (EB-CBT)
What It Is: A specialized CBT program developed by NIMH that gradually exposes children to frustration triggers while teaching coping strategies.
Does It Work?
Pilot studies show 40–60% of kids improve, with reduced outbursts and irritability (ScienceDirect study).
Side Effects: Temporary stress during exposure tasks.
Best for Ages: 8–17.
Resources:
3. Dialectical Behavior Therapy for Children (DBT-C)
What It Is: An adaptation of DBT that teaches children mindfulness, distress tolerance, and emotional regulation, with strong parent involvement.
Does It Work?
Studies show DBT-C reduces irritability and improves family functioning (TPC Journal).
Side Effects: Emotional discomfort during skill-building.
Best for Ages: 7–12.
Resources:
4. Parent Management Training (PMT)
What It Is: A parent-focused approach that teaches reinforcement strategies, consistency, and de-escalation techniques.
Does It Work?
Evidence suggests PMT reduces disruptive behaviors by 70–80% in related disorders, with smaller but meaningful gains in DMDD (Springer study).
Best for Ages: 6–12.
Resources:
5. Medications
Stimulants (e.g., methylphenidate, amphetamines)
Useful when ADHD is also present. Can reduce impulsivity and irritability but may worsen symptoms in some children with ASD (PMC study).SSRIs (e.g., citalopram, sertraline)
Sometimes used for irritability or anxiety but carry FDA black-box warnings for suicidality in youth (Cleveland Clinic: DMDD).Atypical Antipsychotics (e.g., risperidone, aripiprazole)
Often used for severe aggression. Risperidone is FDA-approved for irritability in children with ASD (ScienceDirect article).Mood Stabilizers (e.g., lithium, valproate)
Less evidence for DMDD. Sometimes considered in complex cases (PMC review).Other medications (atomoxetine, amantadine, anticonvulsants)
Studied in smaller trials or case reports with mixed results (ERIC case study).
6. Multimodal / Combined Approaches
What It Is: Uses therapy, medication, school supports, and lifestyle changes together.
Does It Work?
Expert consensus suggests multimodal care works best, with 70–90% improvement in DMDD cases when ADHD is also present (Frontiers Delphi Consensus).
Resources:
DMDD and ASD: What’s the Connection?
DMDD and ASD can occur together, making treatment more complex. Outbursts may come from mood dysregulation (DMDD) or sensory overload (ASD). This overlap increases the risk of misdiagnosis, so a thorough evaluation by a child psychologist or psychiatrist is essential. Treatments like CBT or PMT can help both, but ASD-specific supports (e.g., sensory therapy, social skills training) may also be needed.
Key Takeaways for Parents
Start with therapy first: CBT, EB-CBT, DBT-C, and PMT are evidence-based and low-risk.
Medication is not first-line: Reserved for severe cases or when ADHD/ASD are also present.
Combination works best: Therapy plus school support and, if necessary, medication.
If ASD is present: Ensure treatments also address sensory and communication challenges.
Stay informed: Use trusted resources and ask your child’s care team questions.
Final Thoughts
Parenting a child with DMDD or DMDD and ASD can be exhausting, but you’re not alone. The treatments outlined here, from therapies to medications, offer hope for managing symptoms and improving quality of life. This guide is designed to help you feel prepared when talking with your child’s care team.
Disclaimer: This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare provider for your child’s specific needs.
contact@specialneedskids.com
123-456-7890
Important: Educational Information Only
Content on this Site is for learning, not medical advice. We do not diagnose, treat, or provide individualized care. Research changes over time; some options are off-label or experimental. Talk to your clinician before starting, stopping, or changing any treatment. In an emergency, call 911.
